Effective Psychological and Behavioural Interventions in Obesity Management
- All obesity management interventions involve behaviour on the part of the individual living with obesity (e.g., eating, activity, medication adherence), so behavioural change supports should be incorporated into all obesity management plans. This requires a shift in the patient-provider relationship from the provider as the expert (teach and tell) to that of the collaborator, sensitive to the psychology of the person.
- Obesity management interventions should be evaluated based on how sustainable the behavioural components of the intervention are for the individual. Obesity management plans that are sustainable for the individual should be prioritized over clinician- or program-led management plans.
- Individuals living with obesity should be encouraged to build self-esteem and self-efficacy (confidence to overcome barriers to the desired behaviour), based on results that are achievable from behavioural efforts and not on idealized ideas of body weight and
- Nutrition, medical adherence and physical activities are outcomes of psychological and behavioural interventions and not interventions in themselves. Behaviour change strategies underlying dietary, medical and activity programs should be identified (i.e., what are the change strategies by which sustainable changes to eating, medical adherance and activity are achieved?)
- Adopt a collaborative relationship with the patient, using the principles of motivational interviewing, to encourage the patient to choose and commit to evidence-based, sustainable behaviours associated with obesity management.
- Consider the use of a minimal intervention tool, such as Obesity Canada’s 5As of Obesity ManagementTM (Ask, Assess, Advise, Agree, Assist).
- Healthcare providers should ask permission to educate the patient about obesity management success being related more to improved health, function and quality of life resulting from achievable behavioural and psychological goals, and not just on the amount of weight loss.
- Education should be focused around biology, bias and behaviour. Ask permission to discuss evidence regarding biological and environmental factors, including genetics (family history, the instinctual drive for food), neuroendocrine functions that promote weight regain following weight loss, and physical and social environments (i.e. built environment, food availability/security, sociocultural factors).
- Consider using the concept of “best weight” (i.e., the weight that a person can achieve and maintain while living their healthiest and happiest life). This education should be offered as a means of reducing self-bias and supporting appropriate outcome goals that acknowledge that weight is not a behaviour. This encourages body acceptance.
- Educate the patient that success is related to setting achievable, sustainable goals to which they can adhere, while developing confidence to overcome barriers and fostering an intrinsic motivation to maintain the plan. Goals should positively impact health, function and quality of life.
- Encourage the patient to:
- Set, and sequence goals that are realistic and achievable.
- Self-monitor behaviour.
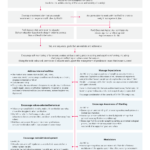
- Analyze setbacks using problem solving and cognitive reframing, including clarifying and reflecting on values-based behaviours. See Figure 1 for an illustration of how to support the patient in their obesity management journey.
- For providers who function within teams (including obesity specialty programs), at least one member of the team should develop competency in behavioural interventions, including self-monitoring, goal setting and action planning, reinforcement management, social comparison, cognitive restructuring, motivational interviewing and values-based counselling. Psychological and behavioural interventions should focus on the impact of the intervention on adherence, self-efficacy and autonomous motivation.
- Multicomponent psychological interventions (combining behaviour modification [goal setting, self-monitoring, problem solving], cognitive therapy [reframing] and values-based strategies to alter nutrition and activity) should be incorporated into care plans for weight loss and improved health status and quality of life (Level 1A, Grade A) in a manner that promotes adherence, confidence and intrinsic motivation (Level 1B, Grade A).
- Healthcare providers should provide longitudinal care with consistent messaging to people living with obesity to support the development of confidence in overcoming barriers (self-efficacy) and intrinsic motivation (personal, meaningful reasons to change), to encourage the patient to set and sequence health goals that are realistic and achievable (Level 1A, Grade A,), to self-monitor behaviour (Level 1A, Grade A) and to analyze setbacks using problem-solving and adaptive thinking (cognitive reframing), including clarifying and reflecting on values-based behaviours (Level 1A, Grade A).
- Healthcare providers should ask patients’ permission to educate them that success in obesity management is related to improved health, function and quality of life resulting from achievable behavioural goals, and not on the amount of weight loss. (Level 1A, Grade A).
- Healthcare providers should provide follow-up sessions consistent with repetition and relevance to support the development of self-efficacy and intrinsic motivation. Once an agreement to pursue a behavioural path has been established (health behaviour and/or medication and/or surgical pathways) follow-up sessions should repeat the above messages in a fashion consistent with repetition (the provider role) and relevance (the patient role) to support the development of self-efficacy and intrinsic motivation (Level 1A, Grade A).
- The main goal of psychological and behavioural interventions is to help people living with obesity make changes that are sustainable, that promote positive self-esteem and confidence, and that improve health, function and quality of life.
- There is not one pathway to success. Goals should be individualized and be important to the individual and not just the clinician or program.
- There are many psychological and behavioural strategies that can be helpful. Individuals living with obesity should seek out a clinician with expertise in behaviour change to help identify relevant strategies.
- Given that healthier weights involve overcoming many challenges (cravings, habits, availability, social pressures) sustained behaviour change is more successful if the behaviours chosen by the individual are consistent with his/her core values.
Figure 1: Solo MD Model